Embark on a comprehensive exploration of the Pharmacology 2019 ATI Proctored Exam. This in-depth guide provides a comprehensive overview of the exam’s content, equipping you with the knowledge and understanding necessary to excel.
Through a detailed examination of drug classifications, pharmacokinetics, pharmacodynamics, adverse drug reactions, drug interactions, medication administration, and pharmacotherapy, this guide unravels the complexities of pharmacology and empowers you to navigate the exam with confidence.
Drug Classifications and Mechanisms of Action
Drug classifications are essential for understanding the mechanisms of action of different drugs and their clinical applications. They provide a framework for organizing drugs based on their pharmacological properties, chemical structures, or therapeutic uses.
Drug classifications can be based on various criteria, including:
- Pharmacological Effects:Drugs are classified based on their primary therapeutic effects, such as analgesics (pain relievers), antipyretics (fever reducers), and antibiotics (antibacterial agents).
- Chemical Structure:Drugs with similar chemical structures often have similar pharmacological properties. For example, opioids, such as morphine and fentanyl, share a common chemical structure and produce similar analgesic effects.
- Therapeutic Uses:Drugs can be classified based on their intended therapeutic uses, such as cardiovascular drugs, antibiotics, or psychiatric medications.
Understanding drug classifications is crucial for effective patient care. It enables healthcare professionals to:
- Select the appropriate drug for a specific condition based on its pharmacological properties and therapeutic uses.
- Predict potential drug interactions and adverse effects based on the drug’s classification and mechanism of action.
- Monitor drug therapy and adjust dosages appropriately based on the drug’s classification and clinical response.
Pharmacokinetics and Pharmacodynamics
Pharmacokinetics and pharmacodynamics are two closely related disciplines that study the effects of drugs on the body. Pharmacokinetics focuses on the absorption, distribution, metabolism, and excretion of drugs, while pharmacodynamics examines the biochemical and physiological effects of drugs.
Absorption
Absorption is the process by which a drug enters the body. Drugs can be absorbed through the skin, the lungs, the gastrointestinal tract, or the mucous membranes. The rate and extent of absorption depend on a number of factors, including the drug’s solubility, the surface area available for absorption, and the blood flow to the absorption site.
Distribution
Once a drug has been absorbed into the body, it is distributed to various tissues and organs. The distribution of a drug depends on its solubility in water and lipids, its binding to plasma proteins, and its ability to cross cell membranes.
Metabolism
Metabolism is the process by which a drug is broken down into smaller molecules. Metabolism can occur in the liver, the kidneys, or other tissues. The rate and extent of metabolism depend on a number of factors, including the drug’s chemical structure, the presence of enzymes that can metabolize the drug, and the drug’s dose.
Excretion
Excretion is the process by which a drug is eliminated from the body. Drugs can be excreted through the kidneys, the liver, or the lungs. The rate and extent of excretion depend on a number of factors, including the drug’s solubility, the drug’s binding to plasma proteins, and the drug’s dose.
Relationship Between Pharmacokinetics and Pharmacodynamics, Pharmacology 2019 ati proctored exam
The relationship between pharmacokinetics and pharmacodynamics is complex. However, in general, the concentration of a drug in the body is directly related to its pharmacological effects. The higher the concentration of a drug in the body, the greater its pharmacological effects.
Conversely, the lower the concentration of a drug in the body, the lesser its pharmacological effects.
Adverse Drug Reactions and Drug Interactions
Adverse drug reactions (ADRs) are unintended, harmful effects of medications that occur during their therapeutic use. Drug interactions occur when two or more drugs taken together alter each other’s effects.
Types of Adverse Drug Reactions
- Type A reactionsare predictable, dose-dependent reactions that are an extension of the drug’s pharmacological effects.
- Type B reactionsare unpredictable, non-dose-dependent reactions that are not related to the drug’s pharmacological effects.
- Type C reactionsare long-term reactions that develop after prolonged drug use.
- Type D reactionsare delayed reactions that occur after the drug has been discontinued.
Mechanisms of Adverse Drug Reactions
- Allergic reactionsare caused by the production of antibodies against the drug.
- Idiosyncratic reactionsare unpredictable reactions that are not related to the drug’s pharmacological effects.
- Toxic reactionsare caused by high levels of the drug in the body.
Management of Adverse Drug Reactions
The management of ADRs depends on the type of reaction. Mild reactions can be managed with supportive care, while more severe reactions may require discontinuation of the drug and treatment of the symptoms.
Types of Drug Interactions
- Pharmacokinetic interactionsalter the absorption, distribution, metabolism, or excretion of drugs.
- Pharmacodynamic interactionsalter the effects of drugs at their target sites.
Mechanisms of Drug Interactions
- CYP450 enzyme interactionscan alter the metabolism of drugs.
- Protein binding interactionscan alter the distribution of drugs.
- Receptor interactionscan alter the effects of drugs at their target sites.
Management of Drug Interactions
The management of drug interactions depends on the type of interaction. Some interactions can be managed by adjusting the dose or timing of the drugs, while others may require discontinuation of one of the drugs.
Medication Administration and Nursing Responsibilities: Pharmacology 2019 Ati Proctored Exam
Medication administration is a critical aspect of nursing practice, requiring knowledge, skill, and adherence to safety protocols. Nurses play a pivotal role in ensuring the safe and effective delivery of medications to patients.
Routes of Medication Administration
Medications can be administered through various routes, each with its advantages and considerations:
- Oral:Convenient, well-tolerated, and suitable for self-administration.
- Intravenous (IV):Provides rapid onset and precise dosage control, but requires sterile technique and close monitoring.
- Intramuscular (IM):Suitable for medications requiring rapid absorption or prolonged action.
- Subcutaneous (SC):Less painful than IM, suitable for medications with slower absorption rates.
- Transdermal:Delivers medication through the skin, providing sustained release over time.
- Inhalation:Administered through the respiratory tract, suitable for pulmonary conditions or rapid absorption.
- Ophthalmic:Applied to the eyes, treating local infections or conditions.
Principles of Safe Medication Administration
Safe medication administration adheres to the “Five Rights” principles:
- Right Patient:Verify patient identity using two identifiers.
- Right Medication:Check medication name, dosage, and form against the prescription.
- Right Dose:Administer the exact dosage prescribed.
- Right Route:Use the prescribed route of administration.
- Right Time:Administer medications at the scheduled time intervals.
Nurse’s Role in Medication Administration
Nurses are responsible for:
- Assessing patient needs and determining appropriate medication regimens.
- Educating patients about their medications and potential side effects.
- Monitoring patients for adverse drug reactions and interactions.
- Documenting all aspects of medication administration, including patient response.
- Reporting any medication errors or concerns to the healthcare team.
Types of Medication Errors
Medication errors are unintentional mistakes that can have serious consequences. They include:
- Prescribing errors:Incorrect drug, dosage, or route prescribed.
- Transcribing errors:Errors made when copying or interpreting prescriptions.
- Dispensing errors:Errors made when filling prescriptions.
- Administration errors:Errors made when giving medications to patients.
Causes of Medication Errors
Medication errors can be caused by various factors, including:
- Lack of knowledge or training.
- Fatigue or distractions.
- Poor communication.
- Inadequate staffing.
- Complex medication regimens.
Strategies for Preventing Medication Errors
Preventing medication errors is crucial and involves implementing strategies such as:
- Using computerized medication systems.
- Implementing bar-code scanning for medication verification.
- Providing ongoing education and training to healthcare professionals.
- Creating a culture of safety and reporting.
- Empowering patients to be involved in their own medication management.
Pharmacotherapy for Common Health Conditions
Pharmacotherapy plays a pivotal role in the management of various common health conditions, aiming to alleviate symptoms, improve quality of life, and prevent disease progression. Understanding the rationale for medication selection, expected outcomes, potential adverse effects, and patient education is crucial for effective pharmacotherapy.
Hypertension
Hypertension, or high blood pressure, is a major risk factor for cardiovascular disease. Pharmacotherapy aims to lower blood pressure, reducing the strain on the heart and blood vessels.
- Angiotensin-converting enzyme (ACE) inhibitors:Block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor.
- Angiotensin II receptor blockers (ARBs):Bind to angiotensin II receptors, preventing its vasoconstricting effects.
- Calcium channel blockers:Inhibit calcium influx into vascular smooth muscle, leading to vasodilation.
Expected outcomes include reduced blood pressure, improved cardiac function, and decreased risk of cardiovascular events.
Potential adverse effects include dizziness, fatigue, and cough (ACE inhibitors and ARBs).
Patient education focuses on lifestyle modifications (e.g., diet, exercise, smoking cessation) and adherence to medication regimen.
Diabetes
Diabetes is a metabolic disorder characterized by elevated blood glucose levels. Pharmacotherapy aims to control blood sugar, prevent complications, and improve overall health.
- Insulin:A hormone that facilitates glucose uptake into cells.
- Metformin:Decreases hepatic glucose production and improves insulin sensitivity.
- Sulfonylureas:Stimulate insulin release from the pancreas.
Expected outcomes include improved blood glucose control, reduced risk of complications (e.g., neuropathy, retinopathy), and improved quality of life.
Potential adverse effects include hypoglycemia (insulin), gastrointestinal upset (metformin), and hypoglycemia (sulfonylureas).
Patient education emphasizes dietary management, regular exercise, blood glucose monitoring, and proper medication use.
Pain
Pain is a common symptom of various conditions. Pharmacotherapy aims to alleviate pain, improve function, and enhance overall well-being.
- Non-steroidal anti-inflammatory drugs (NSAIDs):Inhibit cyclooxygenase enzymes, reducing inflammation and pain.
- Opioid analgesics:Bind to opioid receptors in the central nervous system, producing analgesia.
- Local anesthetics:Block nerve conduction, providing localized pain relief.
Expected outcomes include reduced pain intensity, improved mobility, and increased quality of life.
Potential adverse effects include gastrointestinal upset (NSAIDs), respiratory depression (opioids), and tissue damage (local anesthetics).
Patient education emphasizes appropriate medication use, monitoring for adverse effects, and alternative pain management strategies (e.g., physical therapy, acupuncture).
Detailed FAQs
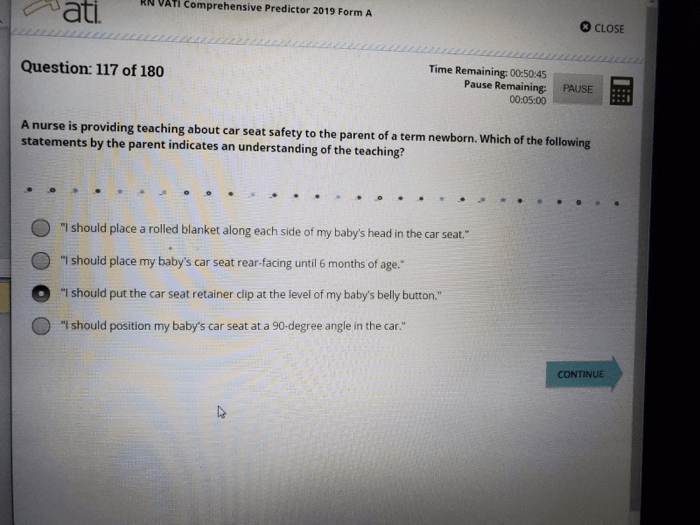
What is the format of the Pharmacology 2019 ATI Proctored Exam?
The exam consists of 150 multiple-choice questions covering the core concepts of pharmacology.
How long is the Pharmacology 2019 ATI Proctored Exam?
The exam has a time limit of 3 hours.
What is the passing score for the Pharmacology 2019 ATI Proctored Exam?
The passing score varies depending on the specific institution or organization administering the exam.